Genital lymphedema may be challenging to diagnose, painful, and embarrassing. It can affect nearly every area of your life. Finding helpful providers and using the right treatments can significantly reduce symptoms of genital lymphedema. But first, providers and the people affected by genital lymphedema must be willing to talk openly about it.
Shelley DiCecco, PT, PhD, CLT-LANA, CI-CS, is a lymphedema therapist and founder of LymphEd. She advocates for removing the stigma around talking about and treating genital lymphedema so people can get the care they need. Dr. DiCecco shares information about genital lymphedema types, symptoms, impacts, and effective therapies.
What Is Genital Lymphedema?
“Genital lymphedema is the accumulation of lymph fluid in any of the genital tissues,” says Dr. DiCecco. “For men, it’s typically external in the scrotum or penis. For women, it can be inside the vagina. It may be internal before it moves to the more visible labia or external pelvic area.”
Types of Genital Lymphedema
There are two types of genital lymphedema, primary and secondary:
Primary Genital Lymphedema
A person with primary genital lymphedema is born with problems in the lymphatic system that prevent proper lymph fluid drainage. The condition may show up at any age, with typical onsets being at birth, puberty, or around the age of 35.
In children, there’s a high association between genital lymphedema and primary lymphedema with gastrointestinal issues. From her experience, Dr. DiCecco also believes, the loss of hormones that occur during menopause can trigger primary lymphedema.
Secondary Lymphedema
The secondary type is acquired and typically occurs due to one or more of these reasons:
- Cancer treatment of the pelvic region, such as colorectal, gynecological, and prostate
- Changes in the body due to pregnancy
- Injury or trauma to the genitals or pelvic area
- Obesity or excess adipose tissue (commonly known as body fat)
Taboos Get in the Way of Diagnosis
Many providers don’t assess for genital lymphedema, so many people don’t know they have it. “It is common for genital evaluations to be limited or skipped altogether. Internal assessment of the vaginal tissue is most often overlooked. Usually, this is due to the comfort and skill level of the clinician and the comfort of the patient. Other limiting factors can include the patient’s age and obesity,” says Dr. DiCecco.
“Unfortunately, in medical schools, we’re typically not trained to do this because general taboos about genitals often carry over into medical practice,” says Dr. DiCecco. How to assess genital lymphedema is scarcely covered in textbooks or training. Most clinicians learn by practicing on each other or model patients with or without genital lymphedema. Rarely do clinician trainees have exposure to genitals or the ability to assess internal vaginal tissue. “So, if clinicians aren’t looking at these areas, they’re not going to see the lymphedema.”
Misdiagnosis or Missed Diagnosis Is Common
Even with a thorough gynecological exam, a provider may miss internal vaginal edema if they don’t palpate (touch and feel) the vaginal tissue. It’s also common for a female to not notice lymphatic-related leakage or discharge due to the common use of sanitary napkins or pads for menstrual and urinary symptoms.
In men, genital lymphedema may be more visible, but it still gets misdiagnosed. “Hydrocele is a condition where the internal structures of the scrotum become swollen, which is a form of lymphatic dysfunction. Hydroceles can lead to genital lymphedema of the entire scrotum or genital region,” says Dr. DiCecco. “It’s appropriate to address hydroceles with the same treatment used with other forms of lymphatic dysfunction, especially compression.”
Genital Lymphedema Symptoms
People with genital lymphedema may experience the same symptoms experienced with lymphedema in other body areas. General symptoms include:
- Bowel and bladder problems such as constipation and leaking urine or feces
- Feelings of pressure in the lower abdomen and pelvic area
- Fluid discharge from the rectum, vagina, or penis
- Numbness in the genital or pelvic area
- Pain with intimacy or intercourse
- Skin and tissue changes, including pubic hair loss, thickening of the skin, discoloration, and skin breakdown, sores, or wounds
Other symptoms associated with genital lymphedema are gender-specific:
Symptoms Women Experience
There is a significant overlap between genital lymphedema symptoms and menstrual cycle symptoms. In addition to general symptoms, women may notice:
- Abnormal vaginal bleeding or discharge
- Pelvic cramping, numbness, or pain that may be dull or sharp
Symptoms Men Experience
Symptoms in men may include:
- Pain and swelling in the penis and scrotum
- Sexual dysfunction, including problems achieving erection (erectile dysfunction) or ejaculation
Impact on Daily Life
“Genital lymphedema can impact an individual’s life in several ways and can even limit interactions with others,” says Dr. DiCecco. The size of the genitals themselves can impact the mechanics of walking, and the noticeable size through clothing can affect mental health.
Other examples of how genital lymphedema can affect daily life include:
- Activity and movement: Genital lymphedema can interfere with activities, even walking short distances, especially due to pain and pressure sensations.
- Leakage: Bladder, bowel, and vaginal leaking can lead to odors and wetness that cause embarrassment. Leakage, particularly urinary, can create a risk of slipping and falling.
- Mental health: Genital lymphedema can impact mental health and make it difficult to maintain a positive body image.
- Sexual dysfunction: Sex can be difficult, painful, or physically impossible, which may impact intimacy and relationships. Learn more about genital lymphedema and sexuality.
- Tissue health: The tissue in the genital region may become filled with lymphatic fluid and thickened or hardened. These changes, along with the warm, moist environment, can lead to skin breakdown, sores, wounds, and infections (cellulitis). They can also cause pain.
“These issues can be debilitating,” says Dr. DiCecco. “Genital Lymphedema can interfere with work and the ability to connect with others. It can lead to people staying home and away from others, especially because the swelling is hard to hide. Women can sometimes hide it by wearing dresses or skirts, but men often can’t. Some men can’t even comfortably wear pants.”
Treatment for Genital Lymphedema
“The genitals are just another body part that has lymphedema, and they deserve all the treatments we offer for other body parts,” says Dr. DiCecco. Essential elements of genital lymphedema treatment include:
Pelvic Floor Therapy
Lymphedema treatment in any area of the body requires exercises because muscle movement moves lymph fluid and helps with drainage. Genital lymphedema is no exception.
“There are over 40 muscles that attach to the pelvis, and often the balance between these muscles is altered,” says Dr. DiCecco. “Exercising the pelvic floor muscles helps with drainage by stimulating or aiding in the ‘pumping’ of lymphatic vessels and nodes in the pelvic area. The contractions strengthen the muscles supporting the organs in the pelvic area to reduce pain, pressure, and bowel and bladder symptoms.”
Both men and women may benefit from working with a pelvic floor therapist. A therapist can minimize or correct these dysfunctions and even perform treatment internally through the vagina and rectum to better address the tissues involved.
Manual Lymphatic Drainage (MLD)
Lymphedema in the pelvic region requires manual lymphatic drainage (MLD). This gentle massage technique assists in moving fluid and particles from the swollen areas to areas with functioning lymphatics to reduce swelling.
“Providers can’t skip over this just because they’re not comfortable with it,” says Dr. DiCecco. “Patients can use MLD clearing of the trunk at home as well. It’s beneficial and relatively easy to perform.”
With genital lymphedema, fluid and particles typically move up the inside of the leg into the lymph nodes in the groin, where it collects. MLD clearing of the trunk involves slowly and gently stretching the skin in the direction you want to move the fluid.
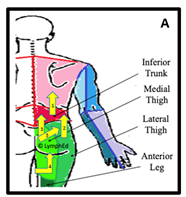
To perform MLD clearing of the trunk from the back (posterior), follow these steps:
- Start by gently massaging the skin on your back towards the axilla (underarm).
- Next, gently stretch the skin on the outer (lateral) thigh/hip, moving in the same direction as step 1.
- Then, proceed at the buttocks in the same direction.
- Last, use the slow, gentle stretch to clear your genital region (scrotum, labia, penis) up towards the buttocks and back. Use a motion as if you’re wiping your bottom.
- Repeat each section 10 to 15 times.
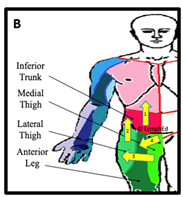
To perform MLD clearing of the trunk from the front (anterior), follow these steps:
- Start by slowly stretching the skin on the abdomen towards the axilla (underarm) or your spine.
- Next, use the same technique on the outer (lateral) thigh/hip going in the same direction as step 1.
- Then, move from the front and inside (medial) thigh over and up through the outer thigh.
- Last, use that same gentle stretching motion in your genital region (scrotum, labia, penis), over into your thigh and then up into your trunk.
- Repeat each section 10 to 15 times.
Diagram A shows the posterior (back) MLD pathway, and Diagram B shows the anterior (front) MLD pathway for genital lymphedema. The yellow arrows represent the direction of fluid flow or drainage. Diagrams provided by Dr. DiCecco.
Compression
“Compression for genital lymphedema during the day needs to be very supportive because these tissues stretch more than tissues of other areas such as the leg or arm,” says Dr. DiCecco. “And nighttime compression is important because that’s when you see the biggest fluid reduction.”
Compression supplies for the pelvic region must be made of breathable materials and should be changed if they become soiled, wet, or sweaty. Moisture can lead to bacterial growth and infections. “It’s important to keep in mind that people need to be able to easily redo their daytime compression themselves, especially if they need to remove it to go to the bathroom,” says Dr. DiCecco.
Skin Care
“The genital area needs to be kept as clean as possible,” says Dr. DiCecco. She advises using wet wipes and allowing the area to dry completely before putting on compression or bandaging.
For sexual intimacy, it helps to incorporate MLD before and after sex. Hygiene after sex is essential for keeping the pelvic area clean to prevent infections.
Intermittent Pneumatic Compression (IPC)
Some intermittent pneumatic compression (IPC) devices, which use air to apply a special compression and release sequence to move fluid in your body, are designed to help with genital lymphedema. However, some pumps don’t directly reduce fluid buildup in the pelvic area. Learn more about the Lympha Press pneumatic pump garments for the lower body that can help people with genital lymphedema.
“If you’re going to use compression with a pump for genital lymphedema, you still need to be doing MLD at home, using compression or bandaging, and doing your exercises,” says Dr. DiCecco. “Pumping can be very beneficial. But if you skip other parts of your home program, especially the MLD clearing of the trunk (at least step 1 above), pumping may make genital lymphedema worse.”
Don’t Suffer in Silence
“Not every provider is a good match. Find someone you’re comfortable with and who’s comfortable examining you ‘down there,’” says Dr. DiCecco. “You need to have providers you can talk to because no one should suffer in silence with genital lymphedema.”
To learn more about genital lymphedema, watch Dr. DiCecco’s webinar on pelvic dysfunction and lymphedema.