People who receive a lymphedema diagnosis often have many questions. Learning about this lifelong condition can empower you to positively influence your health choices and improve your quality of life.
“I think people need to know what’s going on in their bodies,” says Karen Ashforth, MS, OTR, CLT-LANA, an occupational therapist who works with people living with lymphedema. “If you understand the lymphedema process and how you got here, you’ll understand what’s possible. Then, you’ll feel more motivated to do your home program and self-care.”
We asked Ashforth what you need to know most about lymphedema. Below is her “All About Lymphedema” guide, including causes, symptoms, complications, and treatments.
What is Lymphedema?
Lymphedema occurs when the lymphatic system is unable to properly move lymph fluid from the tissues to the lymph nodes to be processed. This lifelong (chronic) condition occurs when lymph fluid builds up in tissues, leading to swelling. Lymphedema can occur anywhere in the body.
Lymph is a clear, watery fluid that protects your body by removing waste products such as:
- Bacteria
- Cancer cells
- Dead cells
- Digestive waste
- Viruses
“The lymph system doesn’t have a central pump like the heart for blood,” says Ashforth. “Instead, it relies on tiny valves inside the lymph vessels that propel the lymph forward. But they only do part of the job. The other part is done by movement of the skeletal muscles.”
Lymphedema Causes
Some people are born with lymphedema, but most develop lymphedema after tissue damage. In some cases, the cause is unknown. Common causes of lymphedema include damage to the lymph system from:
- Diseases such as vein disease
- Trauma, including surgery or radiation for cancer treatment
Types and Stages of Lymphedema
Although there are many causes of lymphedema, there are only two types:
- Primary lymphedema: This hereditary form of lymphedema can begin at birth or develop at any point during a person’s life.
- Secondary lymphedema: This type of lymphedema is caused by a disease or physical trauma.
Some people have both types. For example, it’s possible to have primary lymphedema from birth and develop secondary lymphedema after surgery or other cancer treatment.
Providers classify lymphedema in stages based on the severity of swelling and symptoms. Stage 0 is the mildest, and Stage 3 is the most severe.
How Providers Diagnose Lymphedema
You may receive a lymphedema diagnosis from your primary care physician or another healthcare provider. Diagnosis typically involves a physical exam and discussion of your medical history, plus:
- Palpation, the feeling of tissue for evidence of swelling.
- Stemmer’s sign, a specific type of palpation that tests the ability of the skin to stretch on the tops of the fingers and toes.
- Pitting edema test, the pressing of swollen skin to see if an indentation remains, indicating fluid accumulation.
- Other imaging tests to determine lymph flow.
Lymphedema Symptoms
In Stage 0 lymphedema, the earliest stage, “there isn’t a lot of visible or palpable swelling,” says Ashforth. “You may only experience a sensation of heaviness or tightness, but it might not yet show up as swelling.”
In later stages, symptoms include:
- Swelling
- Heaviness
- Tightness
- Pain
Lymphedema Impacts on Function and Mobility
In addition to symptoms, lymphedema swelling can hinder movement. “Someone may have swelling in their legs that interferes with mobility,” says Ashforth. “Or someone who has breast cancer-related lymphedema may have swelling in their torso and arm. Upper extremity swelling can prevent them from reaching things on shelves because it limits their range of motion.”
Complications of Lymphedema
When lymphedema progresses, it can lead to complications. Ashforth describes two common lymphedema complications:
Cellulitis
Cellulitis is a bacterial infection that requires treatment with antibiotics because it can develop into a life-threatening infection.
People with lymphedema are at very high risk for developing cellulitis. “This increased risk is because one of the functions of the lymph system is to rid the body of bacteria,” says Ashforth. “You might have bacteria that entered through a small wound that turns into an infection because the lymph system isn’t moving the bacteria to lymph nodes where it can be processed.”
Fibrosis
“Fibrosis is a condition where normal healthy tissues become hardened or thickened,” says Ashforth. “Fibrosis can aggravate lymphedema, and lymphedema contributes to fibrosis.” There are several types of fibrosis, but people living with lymphedema typically experience lymphostatic fibrosis.
Lymphostatic fibrosis develops when swelling isn’t properly decongested, creating a high concentration of cellular waste. The body responds by creating fatty tissue. However, this fatty tissue isn’t soft and spongy like typical body fat. Lymphostatic fibrosis becomes harder and denser, which can restrict movement and further block lymph flow.
Lymphedema Treatment and Management
Early diagnosis and treatment for lymphedema are critical because later stages impact well-being and come with significant risks of complications. “My goal with every patient living with lymphedema is to prevent progression,” says Ashforth. “With each stage of progression, management becomes more challenging. The symptoms and potential for infections, wounds, disfigurement, and debility also worsen.”
Lymphedema treatment consists of four different types of treatment done over two phases. Ashforth details these phases and treatments:
Phases of Lymphedema Treatment
The lymphedema treatment and management phases are:
- Reduction phase: In this intensive treatment period a lymphedema therapist works with you several days a week to get the swelling down.
- Maintenance phase: After the reduction phase, you continue treatment independently with occasional visits to your lymphedema therapist.
Four Main Components of Lymphedema Treatment
Complete decongestive therapy (CDT) is a program of treatment for lymphedema. The reduction and maintenance phases both utilize all CDT treatments, which include:
- Manual lymphatic drainage (MLD): This type of decongestive massage directs lymph fluid from the swollen areas toward lymph nodes, where your body can break it down. Intermittent pneumatic compression (IPC) devices can be very helpful for decongestion, especially for those who have difficulty performing it on themselves.
- Compression: In the reduction phase, a therapist wraps swollen areas with multiple layers of padding and short stretch bandages to contain and reduce swelling. In the maintenance phase, most people wear graduated compression garments to help control swelling.
- Physical activity: Exercise and movement help your body pump lymph fluid away from swollen areas to the lymph nodes. Exercising in water is especially effective because water acts as natural gradient compression to help move fluid.
- Skin and nail care: Lymphedema comes with a high risk of infection that can easily lead to cellulitis. Keeping skin and nails moisturized and free of cracks, wounds, and sores reduces this risk.
Education is Also Key
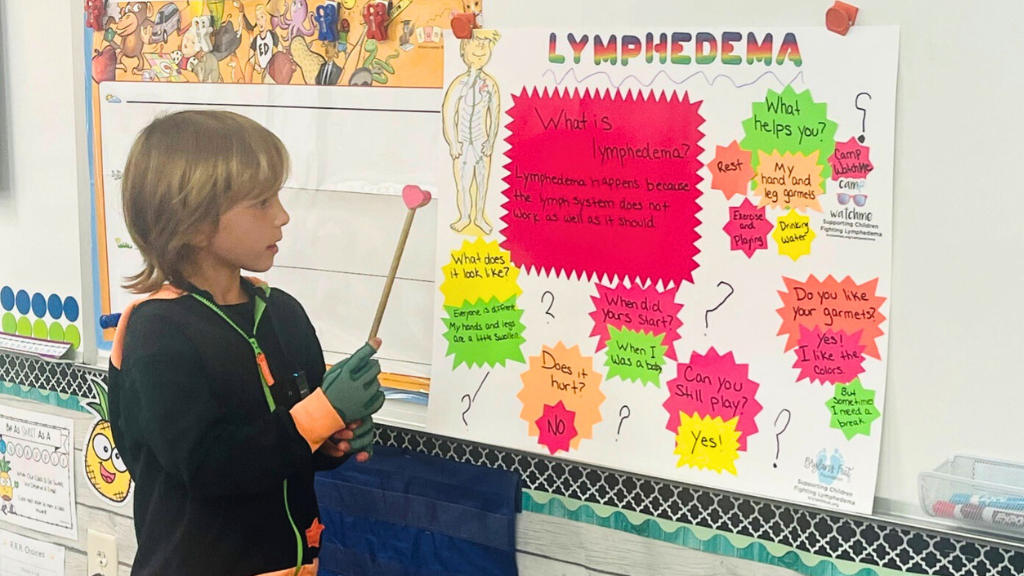
“In addition to the four main components of CDT, I believe that education is a critical fifth component,” says Ashforth. “Understanding lymphedema and your treatment options empowers you to maximize outcomes and improve your quality of life.”
Lympha Press IPC Options
An IPC device uses a sleeve connected to a pump, which applies sequential pressure to help the lymph drain from a swollen area. “I find that most of my patients who try IPC absolutely love it because they feel so much better afterward,” says Ashforth. She says people are often willing to use their pumps multiple times a day because it’s easier than doing self-massage.
Size-inclusive Lympha Press IPC garments and devices are available by prescription, and your device is customized to you with the correct fit and amount of pressure. Lympha Press provides garments suited to swelling anywhere in the body:
- Upper body options: ComfySleeve, Lympha Jacket™, and other arm and upper body garments.
- Lower body options: LymphaPod®, Lympha Pants™, and other leg and lower body garments.
Early Diagnosis and Treatment are Critical
When lymphedema remains undiagnosed, symptoms progress and often worsen. Starting treatment as early as possible slows lymphedema progression and lowers the risk of serious complications such as fibrosis and infection.
Ashforth emphasizes the importance of having hope when living with lymphedema. “Even though lymphedema is a chronic, progressive condition, I believe it’s possible to halt progression and even put it in remission,” she says. “It’s possible to control symptoms through clinical and self-treatment.”
Lympha Press IPC devices help people live better with lymphedema. Learn about the advantages of our innovative pneumatic compression garments designed for home use.