This is a 13-minute read.
By M. Mark Melin MD, FACS, RPVI, FACCWS and Heather Hettrick PT, PhD, CWS, AWCC, CLT-LANA, CLWT, CORE
One of the leading causes of lymphedema is LOVE, or Lymphedema of Venous Etiology. It typically arises from chronic venous insufficiency. Lymphedema can also arise from genetic components and due to damage to the lymphatic system from injury, tumors, surgical procedures, or cancer treatment, including radiation therapy.
In this article, we’ll examine how LOVE impacts patients in terms of wounds, amputations, organ damage, and chronically uncontrolled lymphedema. We’ll also discuss why it’s important to take an integrated approach to lymphedema treatment.
Running a Robust Diagnostic Checklist
In clinical settings where lymphedema may eventually be diagnosed, it’s important to run a full checklist and ensure nothing is missed within the diagnosis. Even while running through things like tobacco use, obesity, diabetes, hypertension, and so forth, never forget about the potential for underlying, clinically silent arterial or venous disease.
Even as a medical professional checks the heart rate, respiration, and blood pressure, they should also be checking the patient’s ankle-brachial index (ABI) to assess for blockages in arterial vessels. Patients need vascular screening as part of routine vital sign assessment when evaluating the causes for lower and upper extremity wounds.
At a wound clinic, we should approach every patient as if they could have lymphatic dysfunction. Consider Dr. Heather Hettrick’s concept that all edema is lymphedema. Excess tissue fluid has the potential to cause lymphatic dysfunction, which can impair arterial perfusion at the microvascular level and contribute to progressive venous dysfunction and wound chronicity.
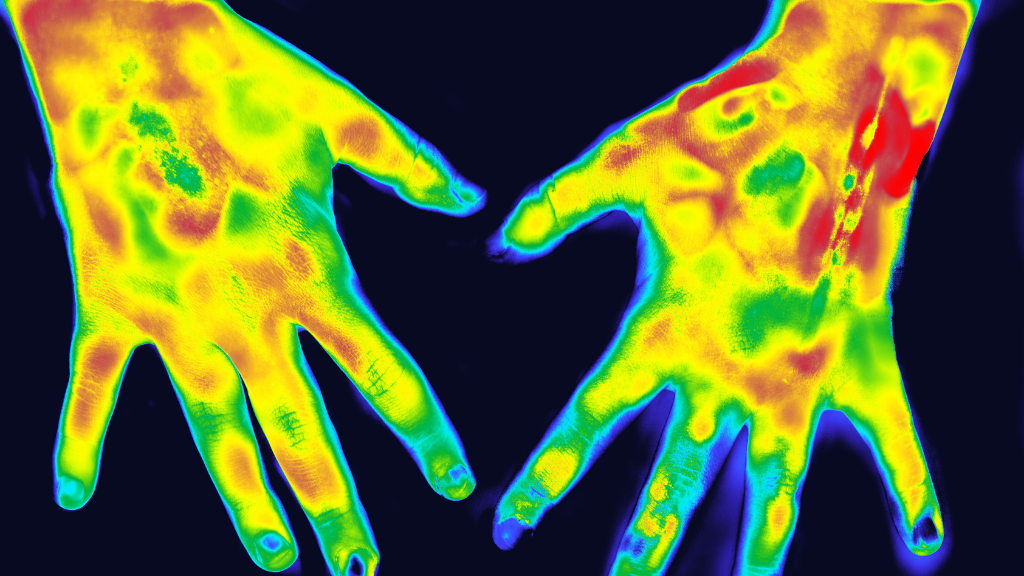
The acronym VAIL reminds us that the Venous, Arterial, Integumentary, and Lymphatic systems (VAIL) are all interrelated. These systems work in unison to maintain the body’s homeostasis where any dysfunction in one system can lead to dysfunction in another interrelated system. The integumentary system is the “structural backbone” to supporting overall functionality; Certified Lymphedema Therapists (CLT) and physicians specializing in Physical Medicine and Rehabilitation (PMR) are experts in integumentary assessment and therapies.
LOVE and Lymphatic Function
Lymphatic function can be impaired in many wounded patients, including people with diabetes.
Lymphedema of Venous Etiology is a result of chronic venous insufficiency, resulting in increased tissue edema due to overloading the carrying capacity of the lymphatic vasculature, resulting in lymphangion dysfunction and lymphatic “backflow” as lymphatic valves fail. Lymphangions can typically carry up to 20 times their normal capacity, though when acutely or chronically “flooded,” lymphangions lose their contractility and normal “forward flow” pumping characteristics. Hence, treating chronic venous hypertension/insufficiency with standard of care vein ablation (thermal or non-thermal/”glue”), foam sclerotherapy, gradient compression, pharmacologic (MPFF, or micronized purified flavonoid fraction), will assist in tissue edema management, restoring microvascular arterial flow that impaired due to chronic interstitial edema that is now known to be lymphatic dysfunction. (All edema is lymphedema; some is reversible, some is not, hence requiring long term therapeutics.)
Interstitial edema occurs in >90% of our patients with chronic wounds. It is now recognized that medications, diabetes, trauma, sarcopenia of para/quadriplegic states, etc., are associated with chronic leg edema that can impair wound healing. This may also be worsened by systemic factors: congestive heart failure, renal dysfunction, liver dysfunction, pulmonary hypertension, sepsis, etc. Recognizing and appropriately treating interstitial edema (which is lymphatic dysfunction) will improve wound healing and outcomes. The local, regional, and systemic causes must all be evaluated and addressed appropriately for treatment.
Due to hyperglycemia, diabetes over time can result in the shedding of the endothelial glycocalyx. This results in the hyperpermeability of the tissue and increased interstitial edema, causing significant skin changes and ulcerations. Recognition of the functional aspects of the endothelial glycocalyx has resulted in a paradigm shift of understanding the importance of lymphatic function in management of tissue edema; the classic Starling function identified that 90% of fluid that flows out of arteries into tissues was reabsorbed into veins. Given the presence of the endothelial glycocalyx as a permeability layer, data now shows that greater than 90% of tissue fluid/edema actually is carried away by the lymphatics, and less than 10% of fluid reenters the veins. This paradigm shift in understanding has greatly increased the understanding of lymphatic importance in the management of venous and lymphatic disorders.
Proper lymphatic function is a restorative and regenerative process allowing cells to maintain fluid equilibrium with their environment. When lymphatic function is compromised, resulting in excess intracellular volume in a single cell, the nucleus can’t work, it can’t produce microRNA, and it can’t accomplish all of the normal things that occur during regular cellular function. When this happens at scale, the result is organ dysfunction.
Sometimes, simple steps can help limit the damage and promote better cellular function. Exercise (such as simple daily walking), improving nutrition, and resolving muscle loss (sarcopenia) are treatments that can help wound patients make progress with managing their conditions.
Diabetes, Compression, and Elevated ABI Readings
When a patient has a high ankle-brachial index (ABI) reading over 1.4, there may be a question about whether compression can be safely applied. It’s crucial to determine whether this result is an accurate or falsely elevated reading before applying compression (patients with diabetes can have falsely elevated ABIs due to arterial calcification). Consulting with Vascular Medicine and Vascular Surgery colleagues can help to clarify any ABI result. A Duplex Ultrasound can also help to define the arterial health of patients with diabetes if the ABI is falsely elevated or “noncompressible.”
In patients with diabetes, there is sometimes a paradoxical improvement in diabetic foot ulcer healing after compression is applied. Treating diabetic foot ulcers is an evolving aspect of the field with many new papers and discoveries in recent years.
Essentially, we are learning that treating underlying lymphatic function works to maximize wound healing. This dovetails with concerns about overcompressing the limbs of people with diabetes and unintentionally worsening their disease, as data is now suggesting that appropriate mild to moderate compression in patients with diabetes with chronic swelling can help accelerate wound healing.
Consider that at least a third of all people in the U.S. have diabetes and of those who develop an ulceration, 25% are at risk of losing a toe or leg. Among those who undergo amputation, there is a 50% mortality within five years and a 40-50% chance that that patient will have an amputation of the contralateral leg within 5 years of the initial amputation. This highlights the importance of proper treatment for people with diabetes and properly diagnosing the underlying contributors to their disease. Maximizing outcomes and quality of life in our patients with diabetes requires a coordinated, integrated team approach. Consider amputation as a failure of proper treatment.
Generally speaking, compression is underutilized. There is a persistent fear about doing too much or too little for someone in a precarious health situation. In the presence of edema/lymphedema, or even when there are no overt signs of edema, there might be a tendency to wait for additional vascular changes before applying treatments like compression. Interstitial edema/lymphedema is often overlooked and underrecognized in the patients with diabetes. However, we believe that compression is one of the missing ingredients that should be utilized more often, more safely, and more effectively. More research is needed in this important area of lymphatic dysfunction in patients with diabetes.
The Brain-Body Connection in Wound Healing
When we care for people with wounds, it’s vital to remember the brain-body connection. Certain vitamins and nutrients that improve systemic function, including the brain, impact how someone copes with and heals from lymphatic disturbances.
Folate, for example, has been shown to impact both depression and wound healing. There’s probably not a single patient in a wound clinic who wouldn’t benefit from more folate or should not at least be evaluated for folate deficiency. Folate should be on the patient assessment checklist for any clinic.
Vitamin D3 should also be on the checklist, along with Vitamin C, B12, and B6. There is evidence that these may help in terms of endothelial nitric oxide production and vasodilation in healing venous ulcers.
Flavonoids, and specifically Micronized Purified Flavonoid Fractions (MPFF; diosmin, hesperidin) are a re-emerging bionutrient that has extensive peer-reviewed, published data regarding improved treatment of lymphedema, venous insufficiency and venous ulcers, and decreasing inflammation. Emerging data suggests MPFF (micronized purified flavonoid fraction) may be an excellent adjunctive component to the standards of care for diabetes management to improve overall outcomes.
Medical lotions (ceramide based creams) and liquids (HOCL, or hypochlorous acid) that lower the skin’s pH have also shown a benefit in wound healing.
Mutually Interdependent Systems
The body’s systems are mutually interdependent, which is a concept that sits at the heart of lymphedema diagnosis and treatment. For a detailed discussion of the VAIL concept, please see Dr. Hettrick’s article, “Is All Edema Lymphedema?” To answer the question posed by the article, yes, all edema is potentially lymphedema, as all edema is lymphatic fluid. This concept falls on a continuum with lymphatic insufficiency on one end, that is a temporary or transient form, compared to the actual disease of lymphedema which currently has no cure, yet remains manageable with proper care and diagnosis.
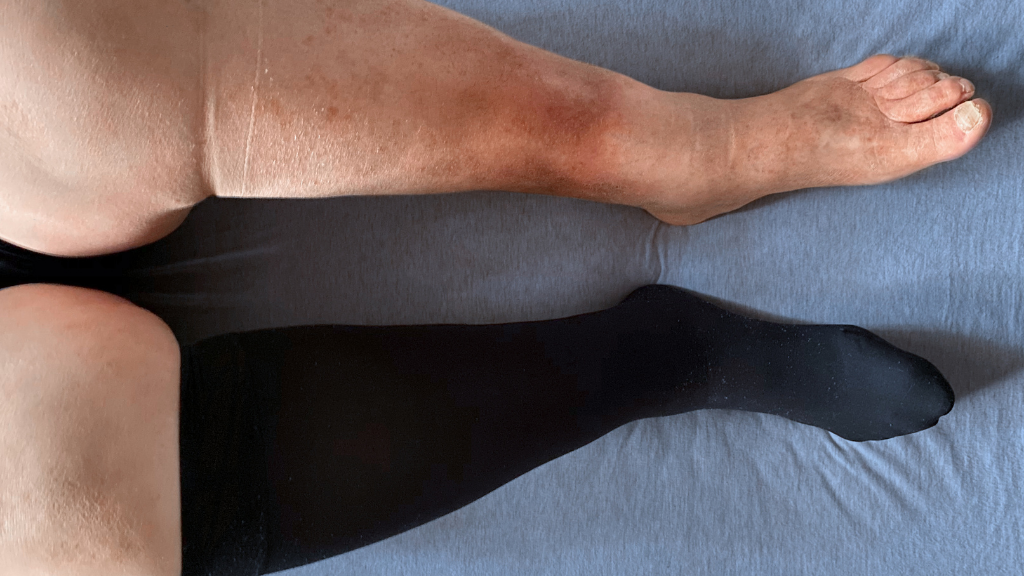
When there is dysfunction in any one of these interdependent body systems, the body’s other systems are at risk of being compromised. When we have dysfunction with the lymphatics, we see on the surface of the body what happens with the skin, such as discoloration, texture changes, wounds, and ulcers. Some patients have a hypersensitive reaction or a propensity for cellulitis (common in venous disease).
With chronic edema, often seen in venous disease, the body contains excess stagnant fluid in the tissues which is caustic, meaning it has a corrosive or abrasive effect. This caustic fluid is filled with the byproducts of metabolic function and senescent cells, enzymes, proteins, pollutants, and toxins. This leads to a chronic inflammatory state, negatively impacting the skin.
It’s interesting to note that when treating patients with chronic venous insufficiency, iron deposits in their skin are noticeable at the outset (hemosiderin staining). During treatment, there is dermal regeneration and an almost lightening of the skin. It would be fascinating to see a full scientific study of this skin lightening phenomenon during LOVE treatment.
Another topic to consider is that of histamines. Many of our patients have very high levels of histamine in their legs. Histamine causes shedding of the glycocalyx, very much like when someone has a cold and develops a red face with swelling and nasal drainage. Histamine also causes shedding of the glycocalyx and can increase interstitial edema due to increased vascular permeability (“leakage”). Steroids applied to the skin may help decrease skin histamine levels; therefore, working with Dermatology may be helpful in management.
The same thing occurs for lymphedema patients, where their lower extremities have increased histamine and hyperpermeability. We’ll see increased redness, swelling, and even what some researchers have called “red leg dilemma syndrome” (British Journal Dermatology, 2019), which is noninfectious but has an elevated histamine level. This is related to the fact that the disease of lymphedema is a chronic inflammatory state.
Knowing this, we can be good antibiotic stewards, and instead of overutilizing antibiotics, we can focus on treating the histamine levels. We can use treatments like steroids on the skin and cover it with saran wrap for an hour a day to show significant improvement and treat the patient’s condition properly.
Why an Integrated Approach is Essential
In summary, always keep in mind that the body, all the way down to the individual cell, wants to heal and remain in homeostasis. In terms of cellular restoration and cellular recovery in LOVE, everyone has the capacity to heal themselves if we provide the right opportunities and treatments.
Treating LOVE takes an integrated approach that avoids the traditional medical silos of diagnosing and treating diseases. While comorbidities are often treated as individual events, everything is linked together in lymphedema.
Lymphedema professionals must take an integrative approach that considers the entirety of the patient from a global perspective. This takes enormous effort and requires significant medical management, but we should never forget that at the center of it all is a patient—a person—who deserves the best possible care.
About Heather Hettrick
Heather Hettrick PT, PhD, CWS, AWCC, CLT-LANA, CLWT, CORE, is a professor, admissions chair, and faculty residency mentor in the department of physical therapy at Nova Southeastern University. She holds a PhD in physical therapy and is a certified lymphedema therapist and certified wound specialist. Her clinical research focuses on integumentary dysfunction, lymphedema, chronic wounds, and venous health.
About M. Mark Melin
M. Mark Melin MD, FACS, RPVI, FACCWS is a graduate of the University of Minnesota Medical School and completed his general surgery residency and vascular fellowship at the Mayo Clinic. He is board certified as both a vascular and general surgeon and practices as a wound surgeon at the South Campus Medical Director of the Wound Healing Institute at M Health Fairview, University of Minnesota.
About Lympha Press
Lympha Press addresses lymphedema with devices that improve lymphatic fluid flow within the body. If you’re a doctor or patient with concerns about lymphedema treatment, please take a look at the innovative therapy options from Lympha Press. Our products offer significant lymphedema symptom relief and are backed by clinical studies.