This is an 11-minute read.
By Heather Hettrick PT, PhD, CWS, AWCC, CLT-LANA, CLWT, CORE
Edema and lymphedema are separate medical diagnoses, but all edema is essentially lymphatic in nature. The medical community and patients with these conditions should know that edema is part of the lymphedema continuum.
In this article, I’ll review the basics of edema and how it relates to lymphatic system overload. I’ll discuss what is meant by the lymphedema continuum, introduce the VAIL concept, and how to use these ideas in clinical applications.
Edema Within the Framework of the Lymphatic System
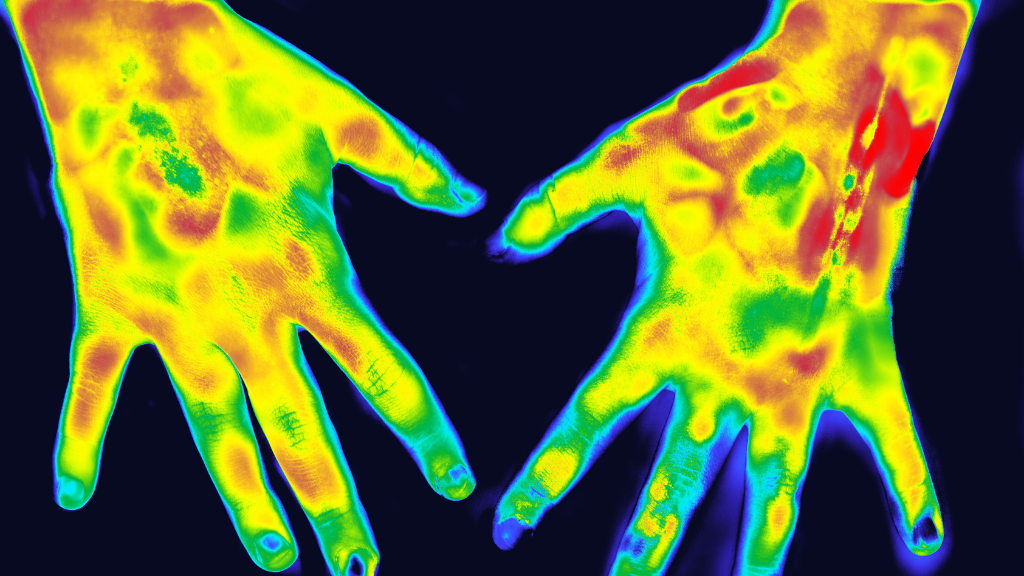
All edema fluid is lymphatic fluid. What does this mean? At the most basic level, edema is swelling of the tissues. When fluid enters the lymphatic capillaries, it’s called a lymphatic load. The lymphatic load is composed of fluid that is partially blood plasma and partially blood plasma proteins. Also involved are the lipid byproducts of wound tissue healing, dead and senescent cells, cancer cells, enzymes, white blood cells, bacteria, endotoxins, and even perfumes, dyes, and pollutants.
There are well over 30 known medical causes of edema; all are associated with the lymphatic system and all involve lymphatic fluid. The various forms of edema are often named according to the area of the body affected.
When edema impacts the lower legs, ankles, and feet, it’s known as peripheral edema. Pulmonary edema is a type that affects the lungs whereas cerebral edema affects the brain. There’s also an older term known as third spacing, which occurs when fluid moves from the vascular system to spaces between the cells or body cavities that normally contain little to no fluid.
A form of edema specific to astronauts is Puffy-Head Bird-Legs Syndrome, which is the result of low gravity or weightlessness. Fluid shifts from the astronaut’s lower body up into their trunk and head, almost like an inverted form of venous insufficiency.
To understand the lymphatic system, consider this analogy. A healthy lymphatic system is like a pickup truck. It has a large transport capacity, so it can handle a big load at any given time. However, what happens when the pickup truck breaks down? Now you’ll have to drive a smaller car with a smaller transport capacity, which requires many more trips. It is still capable of transporting but it is not as efficient and the load can build up. If the smaller car gets damaged, it is now unable to handle its regular smaller transport capacity. The car becomes non-functional and cannot handle any transport capacity.
This analogy illustrates why disease, injury, or surgery creates such a problem for the lymphatic system. When someone has congestive heart failure or postoperative edema, the lymphatic system becomes temporarily overwhelmed. The edema forms transient lymphedema that overwhelms the lymph transport capacity for a period of time but not permanently. If the system is not able to manage the influx of fluid or it is physically damaged or impaired, this leads to the disease we all recognize as chronic lymphedema.
Introducing the VAIL Concept
The VAIL concept is based on the idea that the body’s venous, arterial, integumentary, and lymphatic systems (VAIL) are all interrelated. Anatomically, physiologically, and biochemically, these systems work in unison to maintain the body’s homeostasis. Dysfunction within one of these systems leads to dysfunction in the other systems, which may manifest subclinically or be overt.
Edema is the clinical manifestation of either an overwhelmed or damaged lymphatic system. An overwhelmed system may present with a temporary and transient form of edema whereas a damaged or impaired system leads to a disease state that is permanent. Whether the lymphatic system is overwhelmed or damaged, they both fall along the lymphedema continuum.
Moreover, when there is lymphatic impairment, this leads to localized areas of compromised skin barrier function, which renders the skin more prone to breakdown and impairments. This is known as lymphatic dermopathy. Disorders of the lymphatic system, whether systemic or localized, can lead to negative outcomes like infection, inflammation, carcinogenesis, and multisystem failure involving the VAIL.
Movement encourages the body’s VAIL systems, promoting healthy fluid flow and system function. This has positive effects on the pumping action of the muscles, the pumping action of nodes near the joints, and the person’s overall vascular health. A functional lymphatic system is essential to long-term health given its role in fluid homeostasis, removal of cellular debris, minimizing inflammation, and maintaining immunity.
The Lymphedema Continuum and a Paradigm Shift
In recent years, there has been a major shift in the medical community’s understanding of lymphedema and Starling’s principle of microcirculation. The previous understanding was that hydrostatic pressure favors the filtration of plasma out of the capillaries and osmotic pressure favors the osmotic movement of interstitial fluid into the capillaries, with 90% returned at the venous end and 10% via the lymphatics.
Today, new research has yielded a fresh understanding of these processes. The endothelial glycocalyx layer (EGL), a gel-like matrix with hair-like projections that extend into the lumen of blood vessels, acts as a molecular sieve via mechanotransduction, to regulate fluid flow and macromolecule movement. This leaves only a diminishing net filtration across the capillary bed.
In 2010, Levick and Michel mathematically demonstrated that there is no net reabsorption of fluid back into the venous side of the blood capillaries. All fluid, proteins, and macromolecules are removed from the interstitium by the lymphatics alone. This is why a damaged lymphatic system is so problematic for the body’s homeostasis and health.
Key Takeaways for Clinical Applications
One of the takeaways from this revolutionary shift in lymphatic understanding is that it’s essential to minimize risk factors that contribute to the development of lymphedema. In particular, let’s focus on the impacts of obesity and venous insufficiency.
With obesity, there is a threshold of a BMI of about 40 at which point lower extremity lymphatic dysfunction can occur. Usually, in patients with a BMI of 40 or greater, doctors will find either primary or secondary lymphedema. Some studies indicate that almost 90% to 100% of individuals with BMIs over 60 have some form of secondary lymphedema.
The risk of negative outcomes can be addressed through weight loss, behavior modification, healthy lifestyles, operative intervention, and reductions in extremity overgrowth. This requires a committed medical team as well as patient involvement and adherence. Unfortunately, sometimes there is so much focus on the obesity aspect of the person’s health that there’s not enough focus on the lymphatic element. The lymphatic element can add a great deal of weight and volume, exacerbating the patient’s obesity condition.
With chronic venous insufficiency, the root issue is the increased venous hydrostatic pressure caused by a disorder in the vein in which the venous valves do not function properly. As the venous return to the heart is dependent on the proper functioning of these valves, this disorder causes blood to pool in the veins and leads to venous backflow or regurgitation. This also leads to increased pressure on the lymphatic structures. Collectively, this can impair calf muscle pump function and lead to edema, skin changes, spider veins, varicose veins, phlebitis, blood clots, ulceration, or eventual pulmonary embolism. It is therefore important to address venous insufficiency at the earliest stages before it progresses.
Now that we understand that edema and lymphedema are part of a continuum, how can we incorporate this into our daily practice?
First, dig deeper to discover the etiology of the patient’s contributing factors for medical management. In plain language, go back to the basics. Get to know your patient, their symptoms, and their medical history, including their lifestyle history.
Seek the answers to questions like:
- What is the geography of the swelling?
- How is their skin? Their nails?
- What is the patient’s vascular status?
- What is the patient’s sensory status?
- What is their functional ability?
- What is their cognition like?
- How is their lifestyle?
- Is this lymphatic insufficiency or true lymphatic impairment?
- What would most benefit this patient?
The key takeaway here is that all edema is part of the lymphedema continuum. It may be temporary or transient that responds through medical management, rest, ice, compression, and elevation. It may be more permanent and is best managed with Complete Decongestive Therapy or CDT. CDT involves skin/nail care, manual lymphatic drainage, compression, and exercise delivered in two phases. In either case, all edema is lymphatic fluid. As a healthcare practitioner, you can approach every edema patient thinking, “All edema is lymphedema.” This keeps you more fully prepared to observe and address underlying lymphatic dysfunction while seeking the best possible patient outcomes.
About Heather Hettrick
Heather Hettrick PT, PhD, CWS, AWCC, CLT-LANA, CLWT, CORE, is a professor, admissions chair, and faculty residency mentor in the department of physical therapy at Nova Southeastern University. She holds a PhD in physical therapy and is a certified lymphedema therapist and certified wound specialist. Her clinical research focuses on integumentary dysfunction, lymphedema, chronic wounds, and venous health. She is also exploring the application of forensic science to the development of chronic wounds, comparative pathology research in sea turtles and humans with papillomatosis, and the role of the lymphatics in weightlessness.
About Lympha Press
For over 40 years, Lympha Press has led the world in innovative pneumatic compression therapy. Lympha Press pumps and garments help patients manage lymphedema, chronic venous insufficiency, chronic wounds, lipedema, and other circulatory conditions in the comfort of home. If you’re a doctor or patient who treats these conditions, please take a look at the therapy options from Lympha Press. We offer devices that provide an array of benefits including decreased pain and symptom relief.