By Linda-Anne Kahn CLT-LANA, NCBTMB, CDT, CHNC
This is a 9-minute read.
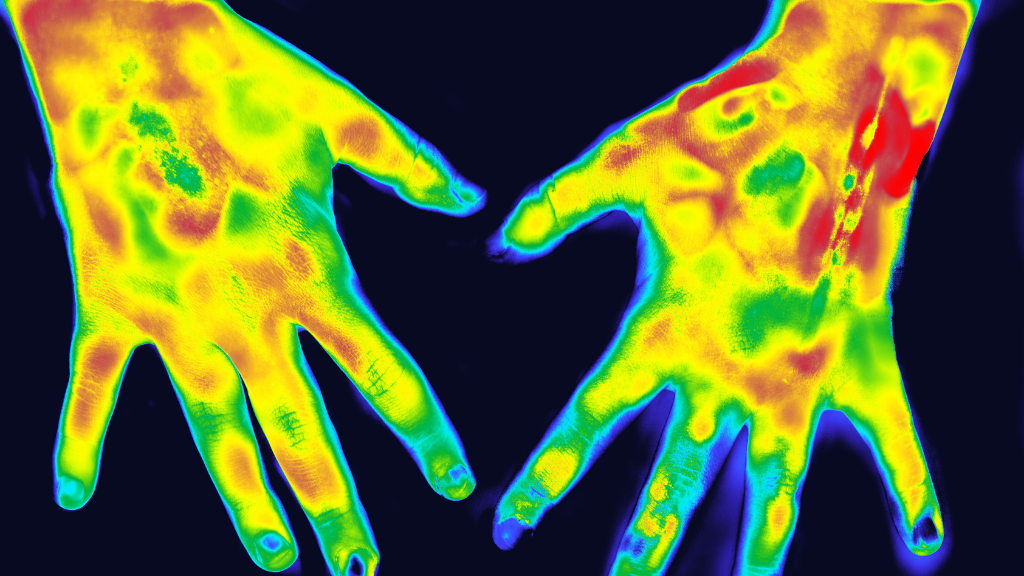
Mast cell activation syndrome (MCAS) is found in 1 in 10,000 to 20,000 people. It involves severe allergic reactions due to the activation of antibodies on the body’s mast cell surfaces, which are found throughout the skin, blood vessels, nerves, and lymph pathways.
Living with the disorder is an ongoing challenge for people with MCAS with repeated episodes of frustrating and sometimes life-threatening symptoms. This article covers the basics of MCAS, plus dietary changes and other treatments recommended for its management.
I’ll also provide details about the involvement of the brain, mitochondria, and glial-lymphatic system. Every day, doctors and researchers are learning more about MCAS. Ultimately, the goal is to help people with MCAS thrive and live successfully.
What Is Mast Cell Activation Syndrome?
Mast Cell Activation Syndrome (MCAS) is a disease of the connective tissue, nervous system, and lymphatic system. It causes severe allergic reactions and anaphylaxis, but its first symptoms are often hives, swelling, low blood pressure, breathing trouble, and bouts of diarrhea.
In MCAS, mast cells are activated to release mediators, which are substances including histamines, proteases, proteoglycans, and cytokines. Certain types of these substances are associated with severe health conditions like cancer and tumors, like the cytokine known as tumor necrosis factor-alpha (TNF-alpha).
When someone has MCAS, they quickly become aware of the condition’s triggers and associated symptoms that make them miserable. Triggers can set off a life-threatening reaction with long-lasting impacts on the body.
For example, someone who previously tolerated a medication well may suddenly develop an MCAS-related reaction that causes swelling, difficulty breathing, and cardiovascular damage. Prescription medications like opioids and antibiotics are known triggers for MCAS, but even something as commonplace as over-the-counter pain relieving NSAIDs, such as aspirin or ibuprofen, can trigger an MCAS episode.
Common MCAS triggers include:
- Stress and emotional pressure
- Sudden temperature changes
- Exercise, including mild to moderate activity
- Being fatigued
- Certain food and beverages, including alcohol
- Prescription, over-the-counter, and illegal drugs
- Perfumes and chemical odors
- Naturally occurring odors in the environment
- Poisons and venoms
- Viral and bacterial infections
- Friction from clothing and shoes
- Mechanical irritation, like vibration
- Sun exposure
Symptoms range from mild and somewhat tolerable to severe and life-threatening. Common MCAS symptoms include:
- Extreme fatigue
- Flushing of the face
- Neck and cheek flushing
- Rashes
- Itching
- Lesions
- Headache that won’t go away
- Heart palpitations
- Abdominal pain
- Bloating
- Diarrhea
- Vomiting
- Uterine cramps and bleeding
- Bone/muscle pain
- Cognitive dysfunction, including brain fog
- Lightheadedness
- Anxiety or depression
In severe cases, the person becomes unable to breathe, walk, or otherwise function normally and may suffer a stroke, heart attack, or other life-threatening health situation. Patients who experience these severe symptoms should call 911 and seek emergency treatment immediately.
Diseases Associated With MCAS
Mast cell activation syndrome is linked to many of the body’s systems and is associated with numerous interrelated conditions. This is why a related condition or disease might be diagnosed before the MCAS diagnosis. MCAS is linked with Dercum’s disease, connective tissue disease, obesity, chronic inflammation, diabetes, and Ehlers-Danlos syndrome.
When Dercum’s disease is present, there is a connection to oxidative stress, obesity, insulin resistance, and/or metabolic syndrome. Dercum’s disease is sometimes diagnosed as fibromyalgia because its signs and symptoms are similar.
You might be surprised to learn that MCAS is also associated with tickborne disease. It can be triggered by many types of insect and reptile venoms, including bee stings, flea bites, mosquito bites, and snake bites.
The Brain and the Role of Mitochondria in MCAS
Brain cells, both neuronal and glial, are susceptible to mitochondrial dysfunction due to their high demand for the energy-carrying molecule adenosine triphosphate (ATP). Brain cells also consume oxygen at high rates, leading to a proportionally high mitochondrial production of reactive species.
There is a known link between mitochondrial oxidative damage and cognitive dysfunction. Reactive oxygen species (ROS) attack tissues and cause damage through oxidation. This impacts the mitochondria, leading to cognitive dysfunction and decline.
Thus, the brain is more susceptible to diseases like Alzheimer’s disease (AD), which is closely associated with oxidative damage. Someone who has AD symptoms should be evaluated for MCAS and Dercum’s disease.
The Lymphatics and Glial-Lymphatic System
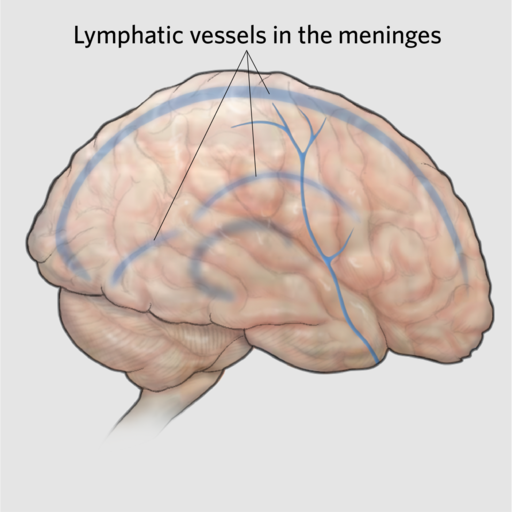
Did you know that we have lymphatics in the brain? This unique drainage system was identified to exist between the cerebrospinal fluid (CSF), brain interstitial fluids, and meningeal lymphatic vessels.
The glial-lymphatic system, also called the glymphatic system, works with the meningeal lymphatic vasculature to improve cerebral drainage. Glial-lymphatic drainage also plays an important role in immune protection and the prevention of central nervous system (CNS) diseases.
This is why new research into brain function reveals insights about aging and the pathogenesis of neurovascular, neurodegenerative, and neuroinflammatory diseases. Your brain’s lymphatic and glial-lymphatic drainage action helps preserve its homeostasis and protect your health.
Treatment Options to Relieve MCAS Symptoms
Patients need to understand that while MCAS symptoms aren’t enjoyable, they’re the result of the body’s natural response to mast cells. Think of MCAS as an overreaction, or what doctors call a secondary activation, due to other external stimuli.
With proper symptom management, many symptoms of MCAS can be significantly controlled. Certain supplements, foods, and lifestyle choices make an impact on the severity of MCAS.
A low histamine diet is often considered the first step in controlling MCAS through the person’s dietary choices. High-histamine foods can trigger MCAS as an allergic reaction by releasing additional histamines into the bloodstream, causing the blood vessels to expand. This can lead to itchy, swollen skin and a dangerous narrowing of the airway.
High-histamine foods to avoid include:
- Aged cheeses
- Alcohol
- Avocado
- Citrus
- Dried fruit
- Eggplant
- Fermented foods
- Legumes
- Processed meats
Flavonoids, enzymes, and mast cell stabilizers are helpful in the treatment of MCAS. These can be found in foods and supplements. Look for anti-inflammatory ingredients including glutathione, N-acetyl cysteine (NAC), alpha lipoic acid, vitamin C, and nicotinamide riboside (NR).
Here are some examples of MCAS-friendly foods that can be incorporated into an MCAS diet under the supervision of a doctor:
- Apples
- Asparagus
- Broccoli
- Cabbage
- Carrots
- Celery
- Cherries
- Cucumbers
- Fresh, non-preserved, and non-reheated meats
- Garlic
- Gluten-free rice, buckwheat, quinoa
- Grapes
- Kale
- Leeks
- Mangoes
- Navel oranges
- Olive oil
- Onions
- Oregano
- Parsley
- Pears
- Peppermint
- Peppers
- Radishes
- Rosemary
- Thyme
- Watercress
- Watermelon
About the Author
Linda-Anne Kahn CLT-LANA, NCBTMB, CDT, CHNC is a lymphedema therapist, an integrative health coach, and the president of Lymphatic Therapy Services of San Diego. She’s an internationally certified manual lymph drainage (MLD) therapist through the Dr. Vodder School in Austria, the Dr. Foeldi School in Germany, and the Dr. Casley-Smith School in Australia. She is a frequent guest speaker at national and international lymphedema and lipedema conferences and is a co-author of the widely-respected book, “The Lymphedema and Lipedema Nutrition Guide.” She is a co-author of the Standard of Care for Lipedema US. She has been treating patients for more than 25 years and is dedicated to helping people thrive and instill confidence in themselves.
About Lympha Press
Lympha Press improves lymphatic flow within the body. Clinicians treating lymphedema, lipedema, chronic venous insufficiency, and chronic wounds should consider Lympha Press therapy options for their patients. Lympha Press at-home therapy is easy to use and offers significant relief with results backed by clinical studies.