By Caroline Fife, MD, FAAFP, CWS, and Missy Baylor, OTR, LMT, CSWS, CLT-LANA
Editor’s note: This article is based on a pediatric lymphedema webinar Caroline Fife and Missy Baylor presented on September 29, 2022. Access this webinar and watch more webinars from the Lympha Press Education Series on YouTube.
This is a 25-minute read.
Understanding the Basics of Pediatric Lymphedema
Recognizing lymphedema in babies and children is a task of pattern recognition. Lymphedema therapists and those who work in wound treatment often have a gift for pattern recognition that allows them to see what’s happening in a child’s body, sparking key diagnostic questions.
To put it another way, you don’t have to know what they have. You just have to know what’s not normal and what questions to ask. This is the first and most important step in determining the proper course of treatment.
Although this article doesn’t take a deep dive into the genetics and heritability of lymphedema in children, it will provide an overview of the imaging and diagnostic criteria. Plus, we’ll provide a closer look at the big picture of pediatric lymphedema, including some food for thought about treating a disease some doctors tend to miss or misdiagnose.
To start, consider a common statistic we hear in the lymphedema field. The mainstream medical literature says primary lymphedema is considered a rare disease that affects only about 1 in 100,000 individuals. That means in the Houston area, there should only be about 23 people with the disease.
However, our Houston practice sees far more than this number of Houston-area residents who are diagnosed with primary lymphedema. Pediatric lymphedema alone represents about 10% of our practice. This leads to the conclusion that the disease must be severely underdiagnosed.
This is a situation that impacts patients and doctors alike. Imagine starting a new practice as a healthcare professional, perhaps thinking you’ll focus on adults with lymphedema. Soon, you discover that your appointments are filled with teenagers, children, and babies. These patients need your help just as much as adults and may even reap more benefits from a lifetime of excellent lymphedema care.
In very young babies, lower extremity lymphedema is most common, but it can happen anywhere in the body, including on the face and genitals. New cases of pediatric lymphedema are being diagnosed at birth, and geneticists are even working to make diagnoses before birth.
The term “congenital” means present at birth, but that doesn’t mean it’s genetic. Most congenital lymphedema does have a genetic link, and some cases are autosomally linked to the chromosomes, with some cases sex-linked and some not. Without going deeper into the complex genetic aspect of pediatric lymphedema, below are a few big-picture takeaways that may help with your diagnosis and treatment:
- Both males and females can be affected.
- The condition can be present at birth and may not be genetic.
- Many cases do have a genetic link, which may or may not be sex-linked.
- Currently, only the most obvious cases are diagnosed at birth due to the presence of clear and observable symptoms, sometimes visible in utero by sonogram.
- Better congenital diagnosis can lead to a lifetime of better care, which shows the importance of understanding the information presented here.
Family Connections at the Point of Diagnosis
Most cases of pediatric lymphedema are diagnosed in teenagers at puberty who are displaying persistent symptoms and are old enough to have developed the language they need to communicate their health problems. Your clinic may encounter a teenager who is describing obvious untreated lymphedema symptoms.
At this point, ask the parents to take off their shoes. It’s time to look at everyone’s feet and see if they display classic lymphedema symptoms like the Stemmer sign. The parents may have undiagnosed lymphedema too.
Consider an actual case history of a healthy teenager at our Houston practice who had previously undergone minor surgery elsewhere for a foot problem. When the teen was six months post-surgery, the incision began to seep what the mother described as an egg yolk-colored fluid. Pressing on the swollen area indicated there was undermining in the pocket.
When this teenager came to our practice, we removed her shoes and observed the Stemmer sign, although her surgeon at the other practice hadn’t noticed it. To us, it was obvious that she had primary lymphedema. Her mother didn’t display obvious signs of lymphedema, and the father wasn’t available for observation.
The simple act of removing the teenager’s shoes and looking for the Stemmer sign could have prevented her post-surgical complications. If the surgeon had realized lymphedema was involved, they may have even reconsidered performing the surgery or created a recovery plan with a CLT.
Imaging Studies on Lymphedema and Related Diseases
As an introduction to lymphedema imaging studies, consider the case of an infant with Milroy disease, a lymphatic disorder of the legs and feet. It’s considered rare and autosomal dominant, which means you can see it in both boys and girls, and it can be identified shortly after birth.
Milroy disease is usually observed to be unilateral in the lower extremities, but it can occur anywhere. Boys may also have fluid in the scrotum. Both boys and girls may display slanting toenails and swelling in the bottoms of the feet.
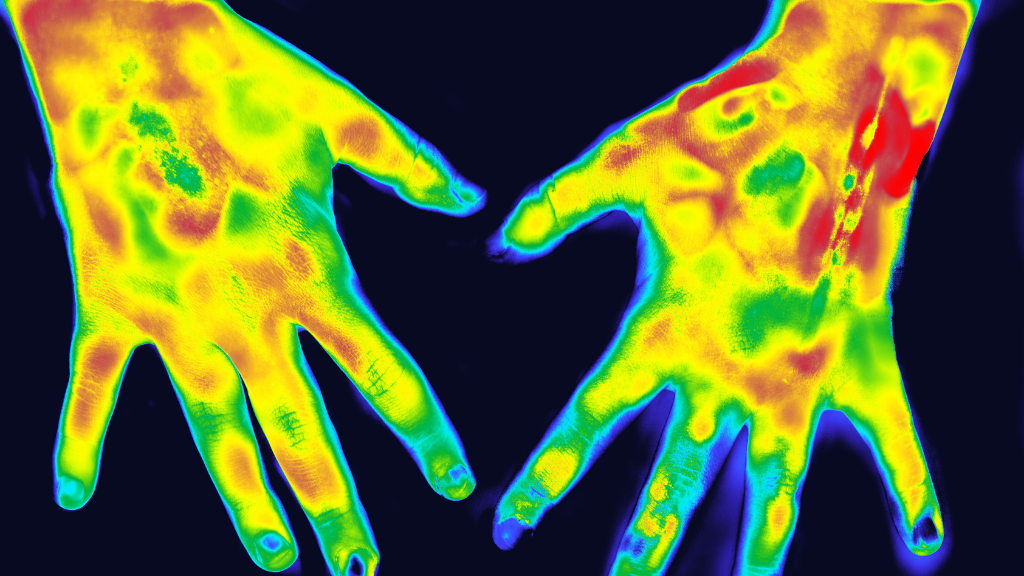
Near-infrared imaging inserts a microdose of indocyanine green (IC green) under the skin of an infant, almost like a tiny bee sting. In real-time, we can watch the lymphangion pumping and see how the fluid moves in the feet and ankles.
I encountered an interesting case of a family with an unaffected dad with imaging studies that looked completely normal. The mother had been diagnosed with lymphedema tarda just beyond her 30th birthday, and her imaging studies showed distinct channels of swelling that looked almost torturous. She’d had an injury on her right leg and had acquired secondary lymphedema, so the dye seemed to spill out everywhere into the individual channels.
Rather than focusing on this case in a genetic sense, think of it more in a familial sense. This mother with lymphedema tarda and secondary lymphedema had two daughters with surprisingly different presentations. Remember, the father was unaffected by lymphedema.
The older daughter presented with unilateral lymphedema praecox as a teenager. A dye injection in her foot showed an almost oozing, lump-like effect, like a spill of coffee without distinct lymphatic channels.
The younger daughter had bilateral congenital lymphedema diagnosed at birth. She had no evidence of distinct lymphatic vessels at all in either of her lower extremity limbs.
Imaging studies can show you when a patient doesn’t appear to have functioning lymphatics, but the concepts that we learn in textbooks don’t always apply to real life. Plus, what we read in textbooks today might not apply ten years from now. As we learn more about lymphedema, we’re realizing it’s more nuanced than we ever imagined.
Another example arises from the world of breast cancer-related lymphedema, which is a large and growing population representing approximately one-fourth of all diagnosed cancers in women. In many cases, even the so-called “normal” side of the body that was unaffected by cancer treatment still has abnormal lymphatics afterward.
Could this mean that breast cancer can trigger the development of lymphedema in a body that didn’t have a normal lymphatic system to begin with? This is the kind of question we should be asking. Again, we should go back to familial and genetic considerations that impact the total health picture of someone with lymphedema symptoms.
A syndrome associated with the lymphatics is known as triple X syndrome, also called trisomy X. In this syndrome, a female has three X chromosomes instead of the usual two. The syndrome impacts the growth of the lymphatic system.
Important things to know about this syndrome include the fact that it occurs in a surprisingly frequent 1 in 1,000 females. Girls with the disorder often look and act normally. You probably know someone who has triple X and neither you nor they realize it.
After an injury or after developing cancer, someone might come to a clinic and have additional genetic testing that shows the underlying existence of triple X. Now they discover they’re genetically predisposed to having other problems like issues with the lymphatic system.
By comparison, consider that Turner syndrome is an example of a syndrome that’s more noticeable and is typically diagnosed at birth or shortly thereafter. The syndrome is associated with the X chromosome, and girls with Turner syndrome often have features like a webbed neck, short stature, delayed or missing puberty, and a lack of development of ovaries and/or breasts.
If you look up Turner syndrome in the National Organization of Rare Diseases (NORD), you’ll see that the authors of NORD articles often forget to include lymphedema as a feature of the syndrome. This shows the conflict between the medical community’s knowledge of lymphedema and its tendency to forget about its association with other conditions.
Staying Alert for Diagnostic Clues
Certain hallmarks of lymphedema are less well-known or are commonly overlooked during the diagnostic phase. As an example, look at the prevalence of unusual birthmarks in people with lymphedema.
Port wine stains are unusual bruise-like permanent birthmarks that are associated with both lymphatic and vascular anomalies. Some people with port wine stains also experience profound problems with lymphedema.
If you see a patient who has a port wine stain, this clue should put you on the alert for other problems that may require follow-up and monitoring. You can’t see a port wine stain in the genetic code, but when you see it on the skin, it can be a clue that your patient may develop cardiac issues or lymphatic challenges.
Another take-home message here is that parents often overlook problems in themselves that they would notice in their children. Likewise, they avoid medical treatment for themselves that they would seek for their children. This is another reason to ask dad and mom to agree to an examination at the same time as the kids.
You may discover that a father who never paid much attention to his swollen feet is displaying profound, yet undiagnosed, lymphedema. He would never have mentioned the problem on his own behalf, but when he saw his daughter’s swollen feet, he immediately sought a doctor’s opinion.
Also, always keep in mind that the obvious existence of lymphedema on one side or extremity doesn’t mean it’s nonexistent on the other side. If you have a child take their shoes off, and it’s obvious that they have lymphedema swelling in the right foot, don’t discount the possibility of lymphedema swelling in the left foot just because it looks more normal by comparison.
Unique Challenges of Treating Pediatric Lymphedema
Bandaging pediatric patients comes with special challenges due to their age and size. A baby or young child may squirm and try to avoid being wrapped in a bandage of any kind. They don’t necessarily understand that they have vascular anomalies or other serious health challenges that make wrapping a medical necessity.
Applying a bandage to a child’s hand or arm can be difficult due to their size and activity level. They may engage in activities that make it easy for the bandages to become soiled or dislodged.
There are also considerations involved with arranging travel to therapy, paying for the therapy, finding a therapist who works with children their age, and finding appropriately sized and fitted garments. The child may need genetic counseling or surgical interventions that would help them tremendously but aren’t necessarily available at your clinic.
Be creative in how you approach and accommodate pediatric patients. At our Houston clinic, we see young patients who have traveled more than 100 miles to arrive at their appointments. They may have language barriers or trouble understanding medical terminology like “manual lymph drainage” or “pneumatic compression.” They may need interpreters, additional time, extra patience, and financial assistance.
Your practice may need to consider providing remote care and taking advantage of technological options that support in-home therapy. Parents are the first line in teaching children about the process of treating pediatric lymphedema. If you teach the parent how to perform manual lymph drainage, they can teach their children and supervise their daily technique as they apply their new knowledge.
It is our experience that children as young as three can be capable of performing simple lymph drainage. Children around this age are usually able to participate with and understand the tools they need for self-management.
Building a Library of Lymphedema Resources
Familiarize yourself with objects, techniques, and stories that children can relate to regarding lymphedema. The classic story of The Three Little Pigs can teach children how to “huff and puff” as a form of diaphragmatic breathing. Pinwheels and blowing bubbles can further engage them in understanding the movement of their diaphragms.
Essential resources for parents, caregivers, and children managing pediatric lymphedema are:
Brylan’s Feat Foundation and its companion Camp Watchme are also two excellent resources for those with pediatric lymphedema. These initiatives can help normalize living with lymphedema and allow children to meet others with the same or similar conditions.
Parents and caregivers can start with these resources, then begin to expand their personal networks of pediatric treatment resources to build a resource library for their children. Create a routine that involves referring to reputable sources and getting good, reliable information about lymphedema care.
Techniques to Help Children Manage Lymphedema
Children respond well to fun tips and tricks that make lymphedema manageable at their level. Focus on demonstrating steps in sequence and establishing a self-care routine that works for their age and ability.
For example, you can use a teddy bear to help the child understand that little bears sometimes need bandaging. Demonstrate where and how the bandage is applied on the bear, then on themselves.
Also, consider that children will be most receptive to learning about their lymphedema at a time of day that feels conducive to therapy. They may be most open to it when they’re not feeling overstimulated and active, so you need to set up a play area in your clinic where they can roam around and get their energy out first.
Other children may be more receptive to receiving manual lymph drainage when they’re playing and somewhat distracted. Parents might dislike seeing their young child playing on a phone or iPad, but a device like this could be the key to settling them down enough for a session of vital lymph drainage.
Approach bandaging as an art unto itself that must be customized to each child and their unique body and situation. Consider yourself an artist who can become proficient in creative bandaging.
As you bandage, think of skin-related issues that apply to children, like limiting skin tears and trauma due to sensitive skin. Consider whether a fabric like terry cloth stockinette might provide a soft touch for a child who is texture sensitive.
Just as with an adult, you need to apply a multilayered sequence of bandages that build compression slowly to get just the right amount of pressure for the child. With smaller children, however, you may have to adapt. Bandaging shouldn’t create unnecessary pressure, immobilization, splay, or deformity that limits a child’s ability to walk or crawl. Look out for any bandaging errors that inhibit the child’s ability to play and move freely.
There’s also an “out of sight, out of mind” aspect of bandaging for very small children who are too young to understand the importance of keeping their bandages in place. You may need to cover their wrappings with a stocking or sock that takes their attention away from the fact that there’s something there to pull on.
Kinesio tape is commonly used in children because most of them tolerate it well, and our practice has found that calling our blue tape “Thomas the Tank Engine Blue” is a great way to help them feel more comfortable with it. If the child likes pink or yellow instead of blue, or a certain cartoon character, adjust your description to fit their preferences.
Pediatric lymphedema patients should be re-measured every four to six months at a minimum because children grow so quickly. If a child arrives at your practice for the first time with rub marks, blisters, or ingrown toenails, consider whether another provider has placed them in ill-fitting garments or bandages that require immediate attention and adjustment.
Older children and teenagers have other concerns, like involvement in sports and activities. If you can make their wrappings look more like athletic support garments, they’re usually happier with them. Our clinic provides athletic team colors that allow our patients to show their team spirit while wearing their compression.
Research on compression pumps increasingly shows that they’re highly effective and can help with pelvic congestion. While it’s not a substitute for traditional therapy, a compression pump can be used in conjunction with children’s daily self-care routines, and we’ve found that most children are accepting of this addition to the therapy regimen. Precautions should be taken to avoid the onset of genital lymphedema if used on a unilateral leg. Using a pantsuit-style pump sleeve is an option, as well as applying external compression to the genital region during the session and after for 30 minutes.
A compression pump can even be used before, after, or during a nap to allow the child to be as comfortable as possible. Of course, a young child should always be supervised while doing so, but this is an example of a method of building a child’s self-sufficiency and autonomy while accomplishing proper lymphedema care.
Final Thoughts on Pediatric Lymphedema
In the late 1990s, lymphedema research was still in its infancy, and women with lymphedema were the unsung heroes pushing doctors forward with developing new therapies and treatments. Even now, the language is just beginning to change from “suffering from” lymphedema to “living with” lymphedema.
Within the medical community, there’s always a lag between what’s happening clinically and what’s being published in books and other materials. There’s also a lag between what doctors know and what they have time to teach their patients. Philosophical changes in any specialty take time.
Some of the things we’re learning from lymphedema imaging aren’t yet widely accessible, so we’re unlikely to see widespread philosophical changes until everyone has access to the imaging results. At the most basic level, we don’t even have names yet for some of the things we’re seeing in the most cutting-edge studies. Again, change takes time.
As the medical community begins to understand the nuances of lymphedema, patients will begin to see the benefits. The patient histories are already providing context that enhances doctors’ understanding of how lymphedema arises and worsens.
You’ll probably learn that some of the things “the book says” aren’t necessarily the patients’ experiences in real life. One of our clinic’s patients said that a drawer fell out of the dresser, hit her leg, caused her swelling, and it had been that way ever since. You might think, “No, the book says that’s not how this works,” but that’s truly how it worked from this patient’s perspective.
Consider a woman who didn’t have radiation during cancer treatment and had no nodal involvement, but still ends up with lymphedema. People may assume it was from surgery and ask, “What did your surgeon do to you?” It doesn’t seem to make sense, but sometimes the lymphatics go awry due to unclear circumstances that don’t fit the textbook definition of having lymphedema.
In summary, all lymphatic systems are not created equally, and we don’t always know this until obvious symptoms arise. We’re living in the 21st century, but lymphedema is still somewhat in the Victorian era in terms of how much we know about it and its diagnosis.
With all of this in mind, we must approach our pediatric patients with creativity, patience, and optimism about their futures. They’re not victims of lymphedema who are just suffering from it. They are survivors who are living and thriving with lymphedema and deserve a lifetime of the best possible care.
About the Authors
Caroline Fife, MD, FAAFP, CWS, received her bachelor’s and master’s degrees from Texas A&M University College of Medicine. After a residency in family medicine at the University of Texas Southwestern, she completed a two-year fellowship in undersea and hyperbaric medicine at Duke University, then joined the faculty of the University of Texas Health Science Center Houston where she served on the faculty for 23 years and became a professor of medicine in cardiology. She is also the chief medical officer of Intellicure, a Texas-based software company, which provides a specialty-specific electronic medical record system to wound and hyperbaric centers. Dr. Fife is the director of clinical research for the U.S. Wound Registry, a nonprofit corporation that provides data for comparative effectiveness studies in wound care and hyperbaric medicine. She is also the medical director of St. Luke’s Wound Clinic in Texas and is the co-editor of Today’s Wound Clinic.
Denise M. ‘Missy’ Baylor, OTR, LMT, CSWS, CLT-LANA, is an occupational therapist who specializes in treating patients with primary and secondary lymphedema, lipedema, post-surgical edema, vascular-related edema, wounds, and similar conditions. She obtained her massage therapy license in 1996 and completed her lymphedema therapy training in 1998 at the Dr. Vodder School in Walchsee, Austria. She earned her Lymphology Association of North America (LANA) certification in 2002, then went on to serve patients at Lymphatic Solutions in Houston and Houston Methodist Hospital Sugar Land.
About Lympha Press
Lympha Press improves lymphatic flow within the body. Clinicians treating lymphedema, lipedema, chronic venous insufficiency, and chronic wounds should consider Lympha Press therapy options for their patients. Lympha Press at-home therapy is easy to use and offers significant relief with results backed by clinical studies.