By Luis López Montoya, PT, Physical Therapy Professor, Research Director at Fi Fisioterapia Integral SC
Luis López Montoya is a lymphedema and physical therapy expert based in Guadalajara, Mexico. His innovation, the Near Infrared (NIR) lymphatic imaging device, is improving the lives of those who wouldn’t otherwise have access to world-class diagnostic technology. The article below is a 5-minute read.
Imagine battling and surviving cancer, only to acquire lymphedema as a post-treatment complication. This is a frustrating situation for many cancer patients who must learn to cope with a new diagnosis of post-cancer lymphedema.
Curiously, some of these patients experience no lymph node removal or damage during their cancer treatment. Instead, it appears that the central venous catheterization-related complications are what led to their lymphedema. This phenomenon captured the interest of myself and my team, and it made us want to investigate further.
Secondary Peripheral Lymphedema From Central Catheterization-Related Complications
Secondary lymphedema is a chronic, progressive disease that causes rich protein edema of the limbs. It often arises due to damage or obstruction of lymphatic structures.
However, secondary peripheral lymphedema may also arise as a complication of central venous catheter procedures. It appears that in some cases patients with venous central catheter complications during cancer treatment may ultimately develop lymphedema even when there has been no lymph node removal.
My team and I observed a clinical case of upper extremity lymphedema as a venous port catheter-related complication. We described the patient’s experience in a clinical report, Lymphatic Injury and Peripheral Lymphedema as Complications of Central Venous Catheter: A Case Report and a Literature Review.
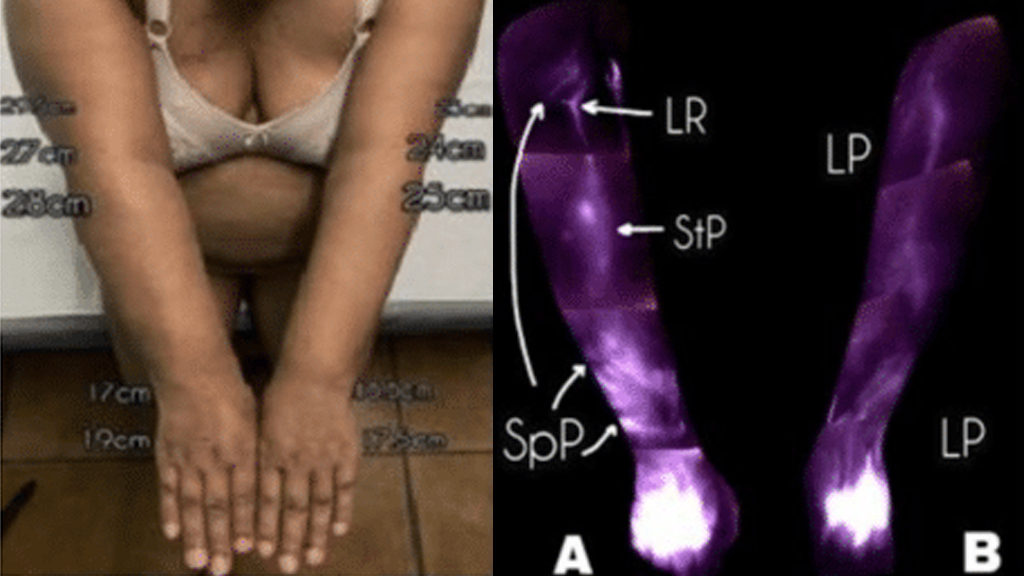
In this case, a 57-year-old woman who had been treated for Hodgkin’s lymphoma in 2019 and 2020 arrived at our facility in March 2021 with a complaint of increased right arm volume. Her situation arose after a right subclavian catheter infection during her previous chemotherapy treatment. She had developed edema that was not improving with rest or elevation and was beginning to limit her movement and daily activities.
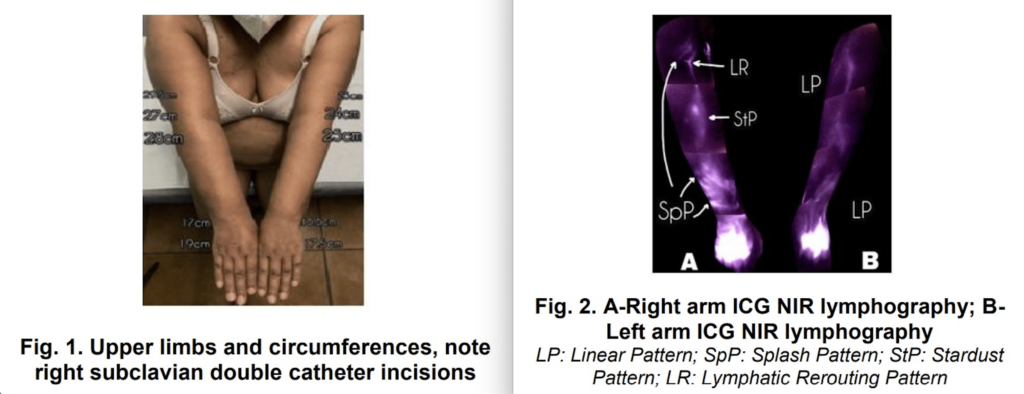
We took her clinical history, did a physical examination, and conducted an ICG NIR lymphography study using the Near Infrared (NIR) lymphatic imaging device I developed. These efforts showed that the patient’s lymphatic system was compromised.
Her edema was progressing in an abnormal pattern that was obvious in the imaging study. When we compared her affected arm to the other arm, we could see that the non-catheterized arm did not show the same lymphedema progression patterns as the affected arm.
The patient’s diagnosis was peripheral lymphedema with evidence of lymphatic detriment as a result of subclavian catheter-related complications.
Catheterization Can Cause Damage to the Lymphatics
To clarify, we can’t say that it is only the insertion of a catheter that can potentially lead to lymphedema. In some patients, there can be infections and complications that come with catheterization such as catheter thrombosis, phlebitis, local catheter infection or thrombophlebitis. There could also be reinsertions and rectifications of the catheter that may impact the patient.
This is why we, as researchers, also conducted a literature review to learn what other researchers and clinicians have already discovered about catheters and lymphedema. We found some reports that make it seem plausible that reinsertion and other factors may play a significant role in the development of peripheral lymphedema, especially in patients with complex conditions or comorbidities.
The bottom line is that catheter-related lymphedema has not yet been extensively investigated. For clinicians, it’s vital to keep this issue in mind, care for their patients accordingly, and do proper long-term follow-ups.
The Importance of Diagnosis and Clinical Literature
Peripheral lymphedema from central venous catheter procedures might not be common, but it’s a clinical reality. It’s a condition that’s underrecognized and underdiagnosed, which puts patients at risk.
This is why my team is publishing clinical literature and issuing a call to others in the scientific and medical communities to do the same. Please share your findings with the world. Peripheral lymphedema from venous catheterization needs much more attention so each affected person may get the diagnosis and treatment they deserve.
About Luis López Montoya
Luis López Montoya is trained as a physical therapist and is a postgraduate professor in physical therapy at several universities in Mexico. In his role as the research director at Fi Fisioterapia Integral SC in Guadalajara, he’s leading a team researching the connections among the fields of lymphology, oncology, vascular peripheral rehabilitation, and physiotherapy. For more than 40 years, Lympha Press has provided innovative compression pump home therapy equipment that supports the best possible patient outcomes.